Dietary fiber produces SCFAs, such as propionate, in the gut and benefits the nervous system and the skin, including neurodegenerative disorders and inflammatory skin conditions such as psoriasis and atopic dermatitis. Gut derived SCFAs, which can be transported to organs throughout the body, have been found to be beneficial to the skin’s barrier formation.
Two sources of SCFAs in the skin exist. Bacteria on the skin and in the gut produce SCFAs. For example, the commensal bacteria of human skin Staphylococcus epidermidis can ferment the major component in stratum corneum, glycerol, into butyrate. This is one reason I formulate many topical products with glycerin – because it’s a prebiotic for commensal bacteria. Let’s look at how the two microbiomes, the skin and gut microbiomes, affect skin health – and brain health!
Back in 2015, when I first heard of the work of Dr. Thomas Schwarz, M.D., at the University of Kiel, using the SCFA butyrate to successfully treat inflammatory dermatoses, I became intrigued and sourced a form of butyrate (a form that doesn’t stink and provides additional benefits) that had been produced by scientists in Trieste, Italia. We found butyrate to be highly beneficial to inflammatory skin conditions, and I began to formulate a number of our products with butyrate. As I defined it in 2018 (Maguire and Maguire, 2018), butyrate is a postbiotic – a molecule produced by bacteria that has benefit to the host. The form of butyrate we use in our products is a synthetic postbiotic – i.e. it’s a modified form of butyrate that the bacteria naturally produce.
Dr. Schwarz and team found that short-chain fatty acids activate resident skin adaptive immune cells, Tregs, the activity of which is diminished in certain inflammatory skin conditions. In other words, Tregs, which control inflammation in the body, could be activated by the SCFA, butyrate. There are a number of factors that can control inflammation in the body, including the skin. For example, ultraviolet radiation can induce Treg which then inhibit cutaneous immune reactions including contact hypersensitivity.
Other studies from the University of Chicago (Cao et al, 2024) have found butyrate, in a form conjugated to serine, to reduce autoimmunity. The form of butyrate we use in our products at NeoGenesis is conjugated to hyaluronic acid. Using this conjugated molecule we provide the benefit of both butyrate and hyaluronic acid to the skin. Cao et al, in their beautiful research paper, sum up the importance of butyrate, and I’ll paraphrase from their paper: Butyrate is derived from the microbial fermentation of dietary fiber in the colon and serves as a primary energy source for colonocytes (cells lining the gut) and maintains intestinal homeostasis. Butyrate is essential for protecting intestinal barrier function by facilitating tight junction assembly (key to preventing leaky gut syndrome). As an epigenetic modulator, butyrate is a histone deacetylase (HDAC) inhibitor and can thus alter chromatin structures and regulate gene expression. Through HDAC inhibition, butyrate has been shown to upregulate forkhead box P3 (Foxp3)—a transcription factor involved in the development and function of regulatory T (Treg) cells (important for anti-inflammation)—as well as suppress NFκB activation (NFkB activation is proinflammatory), inhibit the production of interferon-γ (IFNγ) and upregulate PPARγ. In addition to its broad anti-inflammatory activity, butyrate affects immune cell migration, adhesion, cytokine expression, proliferation, activation and apoptosis. Apart from HDAC inhibition, butyrate can also exert anti-inflammatory effects on immune cells, such as dendritic cells (DCs) and Treg cells, by signaling pathways through specific G-protein-coupled receptors: GPR41, GPR43 and GPR109A. Cao et al found concurrent upregulation of CTLA-4 (CTLA-4 inhibits T-cells) on T cells and downregulation of CD86 (CD86 upregulates T-cells) on myeloid cells can synergistically contribute to a more profound suppression of immune activation, ultimately dampening autoimmune responses. Collectively, these properties of butyrate hold promising potential for the development of therapeutic strategies, particularly in the treatment of immunological disorders, including autoimmune diseases.
Considering the gut microbiome, Dr. Chaogu Zheng, Ph.D., professor at the School of Biological Sciences at The University of Hong Kong (HKU) has found that propionate, a short-chain fatty acid (SCFA) produced in the gut, strongly suppressed neurodegeneration in animal models of Parkinson’s disease (PD) by regulating interorgan signaling between the intestine and brain. I’ve previously published the importance of maintaining gut health to prevent neurodegenerative diseases, including the importance of SCFAs, preventing leaky gut, and maintaining the health of the nutrient-absorbing microvilli.
And relevant to the skin, dietary fiber and SCFAs improve epidermal barrier integrity, thereby limiting early allergen sensitization and disease development. Of note in the study by Trompette et al (2022), is the ability of butyrate to alter lipid metabolism in epidermal keratinocytes, particularly following allergen-mediated skin injury.
There’s been quite a buzz about mucus-eating bacteria in the media. And one tech company has received extraordinary amounts of investment to bring out a supplement based on these bacteria (Akkermansia muciniphila). However, if you read the studies underlying company hype, the mucus-eating bacteria did not lead to significant changes in visceral adiposity and body mass index, the primary objectives of the study. Their results also demonstrated that the supplementation with either Pasteurized A. muciniphila or Alive A. muciniphila did not affect the overall structure of the gut microbiome. This finding is consistent with previous data obtained in rodents, finding that the gut microbiome from mice supplemented with alive A. muciniphila was not significantly modified. Other studies have found that prebiotics work better than probiotics to benefit the gut’s microbiome and measures of obesity. This is uncontrolled capitalism at work – distort the science for the benefit of profits to the rich investors. On the other hand, social democracy, where the people’s money funds scientific research at the universities, yields scientific data on which companies, if they choose to be honest, can make informed decisions about the products they bring to market. Many companies, including mine, do our best to make products that are informed by quality science. Unfortunately, their are some companies, often VC- or private equity-backed (see, for example, Morgenson, Leopold, Karma, and Mazzucato), that look for a quick buck through hyping the science. Some of these are pump and dump schemes, of which Ubiome was one – are a fraud.
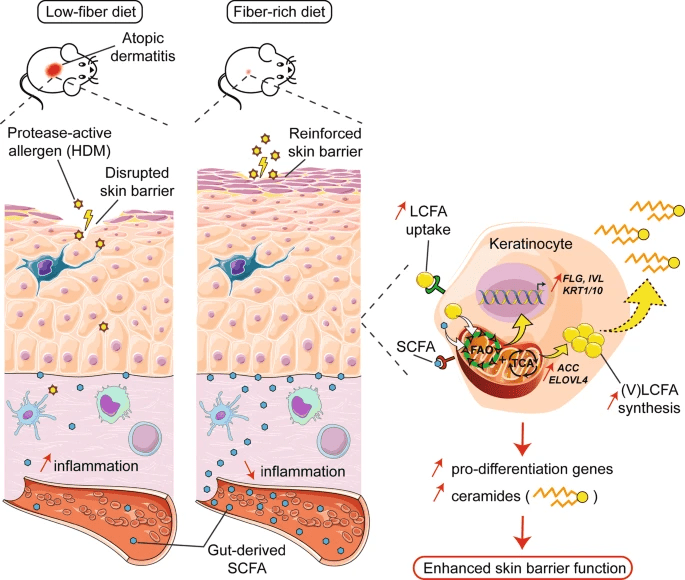
From Trompette et al (2022)
In light of the data provided by Trompette et al (2022) on the cutaneous barrier, as well as work from others in the gut, the fact that mucus-eroding bacteria are less efficient at producing SCFA, particularly butyrate, further puts the epithelial barrier at risk in dietary fiber-deprived individuals. Importantly, the findings are not not just important to skin and brain. Indeed, a deficiency in the high-butyrate-producing bacteria has also been implicated in patients with Crohn’s disease, a disorder that also results from epithelial barrier impairment.
Polyphenols are important too. Polyphenols from vegetables can increase the abundance of Lactobacillus and Bifidobacterium, while inhibiting the abundance of Clostridium. Polyphenols have potent antioxidant benefits. This is great for strains like Akkermansia muciniphila, which thrive in oxygen-free environments and are at risk from free oxygen radicals.
The bottom line, is eat well to provide your gut the needed fibers and polyphenols it needs to create a balanced and healthy microbiome. Your skin will be healthier. Instead of an overhyped probiotic that results in a lot of dead bacteria in your poop, eat lots of vegetables such as oats (fiber) and oranges (polyphenols) to develop a healthy microbiome.