The skin barrier in the epidermis is constantly exposed to microbes and their products. The role of microbes in itch generation was previously unstudied. Deng et al (2023) find that Staphylococcus aureus, a bacterial pathogen associated with itchy skin diseases, directly activates pruriceptor sensory neurons to drive itch.
When the scientists injected MRSA, a type of S. aureus, under the skin of mice, as expected, the mice itched so much that they damaged their skin. But the authors claim to have measured no inflammation associated with the injection. This provides evidence that inflammation is not required for itch to occur.
Instead, research has found that when S. aureus invades the skin, it releases 10 different enzymes, or proteases. One of them, called V8, binds to a protein on nerve cells called proteinase-activated receptor 1, or PAR1. Activation of PAR1 likely starts a chain reaction from the skin neurons, to the spinal cord, and to the brain, which then triggers the urge to itch. In the mouse model used by Deng et al, the itching stopped when researchers used Vorapaxar, a drug that blocks the PAR1 receptor. This may not be the only mechanism by which itching occurs, but this is an important new discovery and gives us much insight into the some of the mechanisms underlying pruritis.
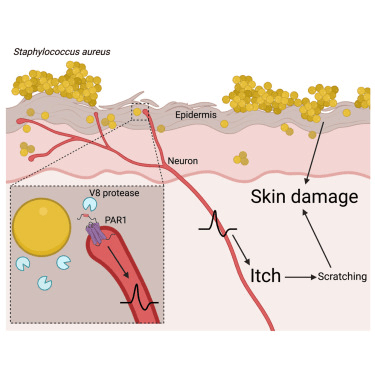
From Deng et al (2023)
As Ogonowska et al (2023) have described, Staphylococcus aureus massively colonizes the skin of patients with atopic dermatitis (AD), and the frequency of detection of multidrug-resistant S. aureus (MRSA) in AD patients is higher than the healthy population, which makes treatment much more difficult.
There’s hope though, and that hope involves using simple, topically applied symbiotic bacteria that are safe and natural to the skin. One set of bacteria are the nitrifying bacteria (Nitrosomonas, Nitrospira, and Nitrobacter), used in NeoGenesis MB-1. The MB-1 product has been on the market since 2015 and is multifunctional – benefiting a number of skin conditions, including acne. As one mechanism of action, Maguire and McGee (2023) hypothesize the MB-1 acts to destroy pro-inflammatory bacteriophage (viruses) associated with acne through a natural CRISPR mechanism in the probiotic bacteria.
These type of nitrifying bacteria in MB-1 have also been found to reduce pruritis and inflammation in humans with atopic dermatitis. Additionally, NeoGenesis is currently testing our second probiotic product that incorporates Bacillus subtilis and Lactobacilli. The bacterium B. subtilis has been found to reduce the S. aureus when topically applied, and Lactobacilli have been found to do the same while reducing the symptoms of AD.
NeoGenesis will have two probiotic products that will be used together in a topical application to renormalize the skin’s microbiome in AD, reduce pruritis, and restore barrier function. Stay tuned.