The modern world’s dramatic increase in the number and types of chemicals in which man is exposed, a major part of of someone’s exposome, responsible for about 90% of diseases (not genetics), is causing a dramatic rise in noncommunicable and communicable diseases. Over 350 000 chemicals and mixtures of chemicals have been registered for production and use, up to three times as many as previously estimated, and an underestimate of the true number of chemical types that have been produced and commercialized. As the skin and other epithelial tissues are compromised and exposed to communicable diseases, skin and epithelial transmitted diseases are on the rise. For example, the shingles virus can enter through the skin or the epithelial tissue in our respiratory tract, and having shingles can even lead to increased risk of dementia (2nd Ref). Further, a compromised skin epithelial barrier caused by environmental factors such as mechanical trauma, exposure to exogenous proteases in microorganisms and our food, detergents, and air pollution can activate the innate and adaptive immune systems, inducing keratinocytes to release pro-inflammatory cytokines and chemokines and enhancing the antigen presentation by intradermal Langerhans cells (LCs) and dermal DCs and activating T-cells. In turn, for example, activation of T2 type T-cells leads to IL-4, IL-5, and IL-13 secretion, provoking skin barrier alteration, immune cell infiltration into skin, and itch as observed in atopic dermatitis.
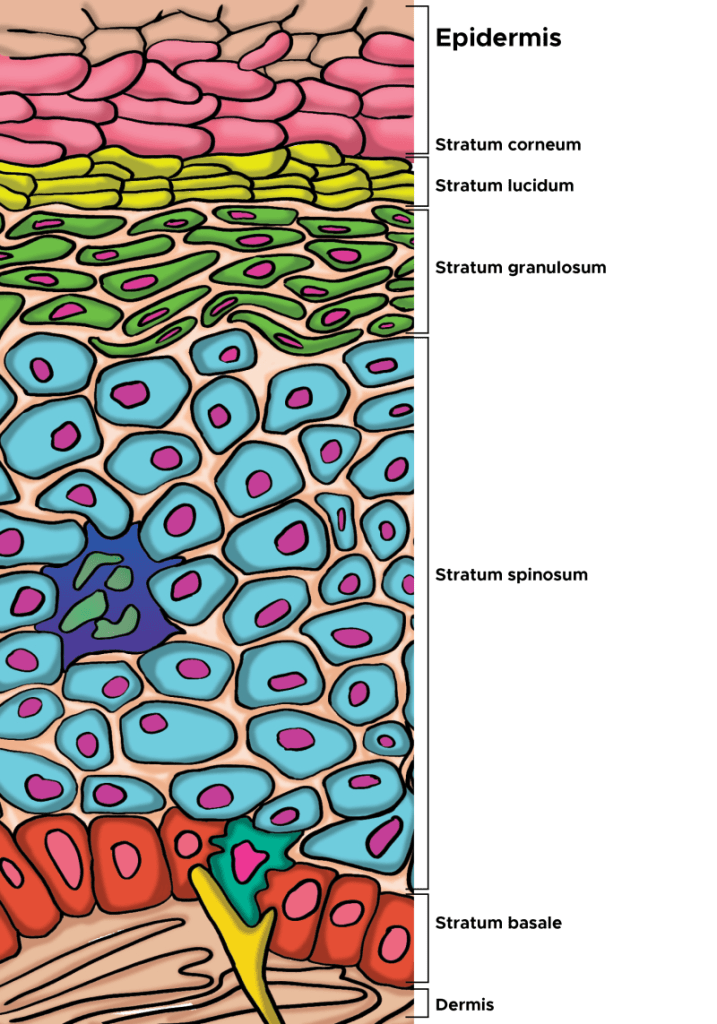
The first essential step to skin immunity is the epithelial barrier, as infection and resulting inflammation are impossible without first breaching it. Epithelia, coated with a sugary glycocalyx, not only comprise our skin but also the mucosal membranes that line our organs. Their ability to secrete squalene, mucus, lipids, and antimicrobials help protect against pathogen invasion. Additionally, epithelia can prevent inflammation by physically shoving out cells infested with toxins, allergens, antigens, pathogens, or other damage by seamlessly extruding them. This is a strategy employed by not only epithelia, but also our hair does the same as it sheds. Given that chronic inflammation could stem from a defective epithelial barrier, the current approach of treating only the inflammation will only partially mitigate symptoms of a more central problem, ongoing wound healing and disrupted barrier.
Scientists now understand that in patients with allergic disease, regardless of tissue location, the homeostatic balance of the epithelial tissue barrier is skewed toward loss of differentiation, reduced junctional integrity, and impaired innate defense and a hyperactive adaptive (trained immunity) immune system. Importantly, epithelial dysfunction characterized by these traits appears to pre-date a predisposition to immunological responses against a range of antigens or allergens, and development of allergic disease.
From the disease perspective, trained immunity is beneficial, as it improves the host’s defense against subsequent infection from pathogens. However, it can also be detrimental and result in overly active immune responses or chronic inflammation. Even the innate immune system has some memory, given evidence that components in House Dust Mite extract activate and likely train macrophages to produce high amounts of CCL17, IL-6, and cysteinyl leukotrienes following re-exposure to HDM through the TNF-α and PGE2 pathways. Thus, an activated immune system, one that has memory and is primed to react, can lead to sensitivities that may be triggered by an overabundance of chemicals in the environment, and those sensitivities heightened by a disrupted barrier.
Evidence that epithelial barrier dysfunction explains the growing prevalence and exacerbations of inflammatory diseases such as eczema has grown through many studies performed world-wide. Diseases encompassed by the epithelial barrier theory share common features such as an increased prevalence after the 1960s that cannot be accounted soley by the emergence of improved diagnostic methods. They are indeed increasing in prevalence, i.e. the number of afflictions per 1,000 people.
Eepithelial barrier dysfunction enables the microbiome’s translocation from the skin’s surface to interepithelial and deeper subepithelial areas, doing in combination with allergens, toxins, pathogens, and pollutants. Thereafter, microbial dysbiosis and possible infection, characterized by colonization of opportunistic pathogenic bacteria and loss of the number and biodiversity of commensal bacteria results. Local inflammation, impaired tissue regeneration, and remodeling characterize the skin that suffers from impaired barrier. For example, commensal bacteria on the skin’s surface are important for epidermal lipid synthesis and improve barrier function. The skin’s microbiome is therefore critical to maintaining epidermal barrier function. The infiltration of inflammatory cells and inflammatory cytokines to affected tissues is part of the immune system’s response to erradicate invading bacteria, allergens, toxins, and pollutants away from the deep tissues. As Peter Elias, M.D. has written, “AD [atopic dermatitis] can be considered a disease of primary barrier failure, characterized by both a defective permeability (Proksch et al., 2006, and references therein) and antimicrobial function.” Further, inflammatory cells and inflammatory cytokines that migrate from the skin to other organs may play roles in the exacerbation of various inflammatory diseases in other organs. Thus, inflammation iniated in the skin may contribute to chronic inflammatory diseases in other tissues.
What Dr. Elias has been saying is that the permeability-barrier abnormality in AD is not merely an epiphenomenon but rather the “driver” of disease activity, an “outside–inside view of disease pathogenesis” (Elias and Feingold, 2001). The evidence for this is: (1) the extent of the permeability-barrier abnormality parallels severity of disease phenotype in AD, (2) both clinically uninvolved skin sites and skin cleared of inflammation for as long as 5 years continue to display significant barrier abnormalities, (3) topical artificial barrier therapy comprises effective ancillary therapy, and (4) specific replacement therapy, which targets the prominent lipid abnormalities that account for the barrier abnormality in AD, not only corrects the permeability-barrier abnormality but also comprises effective anti-inflammatory therapy for AD (Figure 1; Chamlin et al., 2002). Thus, inflammation in AD may begin with insults from without, i.e. the exposome.
That barrier insult can then activate epithelial cells in the skin, keratinocyes, which are non-professional immune cells, but do possess MHC-II molecules, that present antigens to professional immune cells, such as T-cells. Thus, with disrupted barriier, the keratinocytes can recognize antigens and present them to the immune system, leading to inflammation. More and more, scientists are discovering how epithelial cells are part of the immune system, regardless in which organ they exist. Key here is to protect barrier function in all of our epithelial tissues, including the skin.
So if inflammatory diseases such as eczema and psoriasis are environmentally triggered and lead to barrier dysfunction and resultant inflammation, what can we do?
First, calm the inflammation. It’s destructive and further degrades the epidermal barrier. S2RM technology (in NeoGenesis Recovery) is great for reducing inflammation, doing so in both the innate and adaptive immune systems.
Second, use a topical product that provides the 3 lipids and natural moisturizing factors that are needed to rebuild normal stratum corneum and barrier function. One product to use is NeoGenesis Barrier Renewal Cream (BRC).
Third, use a product that provides instantaneous barrier function and commensal bacteria. The instantaneous barrier allows the BRC to rebuld the natural barrier function over time, and the commensal bacteria help to rebuild the barrier through activation of lipid synthesis by skin cells. The commensal bacteria in Neogenesis MB-2 also help to reduce the Staphylococcus aureus infection often assicated with disrupted barrier function.
So remember, these inflammatory skin conditions are triggered by the environment. Therefore, their treatment and prevention means that if you change your environment, you can prevent or treat these diseases. Part of changing your environment is the careful choice of topical products to reduce inflammation and renormalize the structure and function of your skin.