NeoGenesis uses Hydroxypinacolone retinoate (HPR), a newer retinoid that is less irritating than tretinoin and has been found to be as effective in vitro at promoting collagen production. HPR is also more stable than other retinoids in the presence of sunlight and air. Unlike retinol, HPR directly binds to the retinoid receptors and is therefore more effective and less irritating than retinol. The efficacy of HPR is similar to retinoic acid. However retinoic acid (tretinoin) can cause significant irritation of the skin, and is available only by a physician’s prescription. Retinoids can provide great benefit to aging skin. In this blog, I’ll explore some of the mechanisms by which retinoids benefit both the epidermis and the dermis. (Christine Preston contributed to this blog).
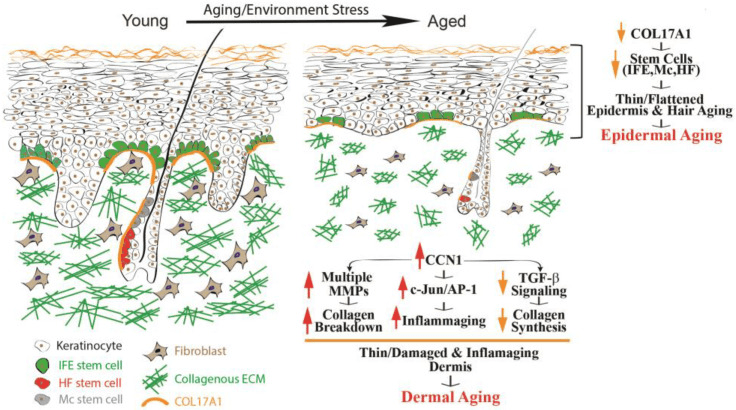
From Quan (2023) Epidermal and dermal aging of human skin. Skin aging includes the thinning of both the epidermis and dermis.
Over time, many alterations occur within the epidermis, collectively known as epidermal aging. These changes in time are characterized by the thinning of the epidermal layer and the flattening of rete ridges (as depicted in Fig 1, on the right). Rete ridges (RR) form an interdigitated surface area that reinforces cohesion between the epidermis and dermis, and this structure demonstrates plasticity, responding dynamically to stimuli such as UV irradiation. RR adapts to disruptions of its boundary during wound repair when cells lose hyper-adhesiveness, allowing the skin to appropriately remodel itself. The principal cause of epidermal aging can be traced to a reduction in the proliferation and turnover of keratinocytes, linked partially to the depletion of interfollicular epidermal (IFE) stem cells and dysfunctional Rete Ridges, leading to poor healing and thinning of the epidermis.
Collagen type, COL17A1 has been of particular interest due to its role in maintaining the homeostasis of the skin stem cells. COL17A1 is a structural element within the dermal–epidermal basement membrane, and it is synthesized by epidermal keratinocytes, not fibroblasts (Xiang et al, 2022). COL17A1 is primarily expressed in the uppermost extensions of the rete ridges area, where the niches for IFE stem cells are located. Research results have suggested a reduction in the expression of COL17A1 in human skin affected by both intrinsic and extrinsic aging factors, including human skin exposed to acute UV irradiation. The decrease in COL17A1 levels within the area specific to the rete ridges can reduce the adherence of IFE stem cells to their designated locations, leading to their removal from the skin. Consequently, the reduction of collagen protein, COL17A1, results in decreased rates of keratinocyte renewal and the development of thinner epidermal layers, the primary morphological characteristic of aging skin.
Human skin has developed two main defense mechanisms to guard against the damaging effects of UV: 1. epidermal thickening, 2. and the stimulation of melanin synthesis, however, photoprotection through increased melanogenesis is more important. As we think about retinoids and what they do for the skin, think about how retinoids help to maintain the normal structure of the skin, can actually thicken the epidermis and dermis, and how important this is for skin function and protection, including protection against UV.
Retinoids, which refer to a group of vitamin A derivatives, are among the most-extensively studied ingredients in skincare for combatting aging and enhancing the appearance of mature skin. Retinoids can stimulate collagen synthesis, inhibit MMP (Matrix metalloproteinases – too much of this activity can break-down proteinaceous tissues) activity, reduce oxidative stress, and modulate gene expression (Quan, 2023). Retinoids have exhibited efficacy in ameliorating the visual manifestations of both intrinsic and extrinsic aging, such as wrinkles, fine lines, and irregular pigmentation. The mechanisms of retinoid’s action may involve the activation of retinoic acid receptors (RARs) and retinoid X receptors (RXRs), which regulate gene transcription and cell differentiation. Retinoids may also modulate the activity of growth factors and cytokines involved in ECM turnover and inflammation. Retinoic acid (RA) is the active form of vitamin A and its precursor is called retinol (ROL). ROL can be converted into its active metabolite within human skin. When retinol is applied topically to human skin, it can penetrate the skin and undergo sequential conversion to retinaldehyde and then to retinoic acid
Skin-equivalent cultures have been used to investigate the regulatory role of retinoids in collagen homeostasis. Typically, these simplified skin constructs feature stratified and differentiated keratinocytes, representing the epidermal layer, layered atop a collagen lattice primarily comprising Type I collagen. Dermal fibroblasts are embedded within this lattice to mimic the dermal layer. When subjected to retinoic acid treatment, these skin-equivalent cultures exhibit a thickened epidermis with a substantial increase in the number of keratinocyte layers and elicit a dermal response akin to the effects observed when retinoic acid is topically applied to human skin in vivo. Consequently, skin-equivalent cultures hold significant potential as a valuable model for delving into the mechanisms by which retinoids enhance the appearance of aging skin in humans.
Increasing the Thickness of the Epidermis and the Vascularity of the Dermis in Aged Human Skin In Vivo Using Topical Retinoids: Stimulating the Growth of Epidermal Keratinocytes and Dermal Endothelial Cells
Topical application of retinoids to aged human skin in a live setting has been found to significantly enhance the thickness of the epidermis by stimulating the proliferation of epidermal keratinocytes, and increasing the number of Rete Ridges. In addition to improving epidermal thickness, topical retinoid has shown a notable increase in the proliferation of endothelial cells and blood vessels in the papillary dermis. These findings suggest that the topical application of retinoids results in the thickening of the epidermal layer and the development of fresh blood vessels within the dermis. The AP-1 transcription factor is critical to enabling the proliferation of keratinocytes in response to growth factors, cytokines, and various stimuli. The AP-1 complex consists of c-Jun and c-Fos, and it has been observed that topical retinoids significantly increases the expression of the epidermal-specific c-Jun protein, leading to a substantial increase in epidermal thickness. There is also evidence that the expression of c-Fos protein increases with retinoid treatment. These findings suggest that topical retinoids enhance the activity of the epidermal-specific c-Jun, and possibly c-Fos transcription factors, thereby stimulating the proliferation of epidermal keratinocytes in aged human skin in vivo.
Topical Retinoids Improve the Dermal ECM Microenvironment by Promoting the Production of Collagenous ECM in Aged Human Skin In Vivo
Topical retinoid treatment increases Type I collagen expression, which constitutes 80–85% of the dermal ECM, while collagen type III constitutes about 8–11%. Topical retinoid also significantly enhances the expression of fibronectin and tropoelastin. In aged human skin in vivo, topical retinoid effectively activates dermal fibroblasts, leading to the substantial production of collagenous ECM through the activation of the TGF-β/Smad pathway, which is a key regulator of ECM production. Topical retinoid administration causes a significant increase in TGF-β1 mRNA expression and a decrease in inhibitory Smad7, while other components of the TGF-β pathway remain unaffected. Additionally, topical retinoid leads to an increase in the expression of connective tissue growth factor (CTGF/CCN2), which is substantially reduced in the dermis of aged individuals and contributes to the decline in collagen production associated with aging. These findings provide evidence that topical retinoid stimulates the production of ECM by dermal fibroblasts through the upregulation of the TGF-β/CTGF pathway in aged human skin.
In addition to the upregulation of TGF-β/CTGF pathway, retinoic acid significantly reduces CCN1 gene expression in both naturally aged and photoaged human skin in vivo. CCN1 is a negative regulator of collagen homeostasis by inhibiting the TGF-β/CTGF pathway and stimulating MMPs’ induction. These data suggest that the mechanism by which topical ROL improves aged skin, through increased collagen production and inhibition of MMPs, may involve the downregulation of CCN1. Thus, retinoids are acting through multiple pathways, inhibiting some and activating others.
In aging skin, decreased vascularity and thinning of the dermis and epidermis are substantial factors contributing to skin fragility and hindered wound healing. Blood flow to the skin, the largest organ in the body, is reduced by 40% between the ages of 20 to 70 years. Topical retinoids not only enhances ECM production, but also improves the dermal microenvironment by promoting the expansion of vasculature through endothelial cell proliferation in aged human skin. An age-related reduction in cutaneous vasculature has been reported. The increased vascularity of the dermis induced by topical retinoids can improve skin blood flow and create a more-favorable microenvironment for the homeostasis of the epidermis and dermis. Further, the promotion of epidermal keratinocyte proliferation and the restoration of ECM production by topical retinoid could create a supportive environment for the growth of endothelial cells and the development of dermal blood vessels. Epidermal keratinocytes are a significant source of vascular endothelial growth factor (VEGF), a powerful factor in promoting angiogenesis. Furthermore, increased production of dermal ECM has been demonstrated to stimulate the proliferation of endothelial cells. As a result, the augmented dermal vascularity facilitated by retinoids may have a significant impact on the homeostasis of both the epidermis and dermis.
Hydroxypinacolone Retinoate (HPR) for Anti-Aging, Photodamage, and Acne
Hydroxypinacolone retinoate (HPR) has demonstrated positive effects as a topical anti-aging ingredient, the authors of the study writing, “Together these data suggest that HPR is an effective alternative to ATRA and other less potent retinoids in the treatment of aging skin without the detrimental side-effects. And the combination of retinoids and salicylic acid can be used to ameliorate the signs of photoaging.
Data have confirmed past studies indicating that topical retinoids are under-used for acne. Further, HPR has been successfully used to treat comedonal-papular, mild to moderate acne of the face. In this study, papain was also used, in addition to HPR, as an exfoliant, and in many cases acne patients may benefit from combination therapies, such as the use of retinoids (HPR) with salicylic acid to better treat acne.
Carotenoids, Like Beta-Carotene, Convert to Retinoids When Topically Applied
You’ll notice on the label of NeoGenesis Skin Restore Serum, that in addition to HPR, carotenoids, including beta-carotene, are included in the product. While topically applied carotenoids absorb into the skin and are converted to retinoids in the skin, the carotenoids also provide antioxidant benefit to the skin. The beautiful yellow color of the vitamin A product, Skin Restore Serum, reflects the yellow pigmented carotenoid antioxidants loaded into the serum.
The amount of carotenoids in the skin depends on dietary intake, and their bioavailability from various foods, with fruits and vegetables as an important source.. After absorption in the gut and transportation into the skin, carotenoids accumulate in the skin, including the adipocytes in the hypodermis. The skin protective benefits of carotenoids, especially from those residing in the epidermis, are many, including protection from UV and air pollution.
Retinoids and Photosensitivity
Photosensitivity to retinoids appears to be a rare event, and quite to the contrary, retinoids have been found to successfully treat some forms of skin photosensitivity. First, let’s dispel the somewhat common belief that topical retinoids enhance UV-induced inflammation. Smit et al (1999) evaluated the minimal erythema dose (MED) for UVB irradiation on topical all-trans RA (tretinoin cream 0.05%) pre-treated skin compared with vehicle cream pre-treated skin and untreated skin. Their study found no significant difference for the MED values either 24 or 48 h after UVB irradiation between the all-trans RA cream treated skin, and the vehicle cream treated skin and untreated skin. In other words, topical retinoid caused no enhanced inflammation when the skin is exposed to UV.
Second, Actinic folliculitis (AF) is a rare recurrent seasonal photodermatosis, relatively newly characterized by nonpruritic, monomorphic pustules and papules appearing 4-24 h after exposure to sunlight. Lesions usually affect the face but also appear on the upper chest and arms. Resolution normally occurs within 7-10 days with cessation of sunlight exposure. AF is resistant to standard treatments used for acne vulgaris and acne rosacea, with only oral retinoids previously being reported as effective. Academic dermatologists in the UK have reported that AF responding extremely effectively to a topical retinoid.
Discussing photosensitivity, be clear that HPA is relatively stable in light and in the air. Applying and using HPA in normal lighting conditions will not degrade the product.
Long Term and Overuse of Retinoids
While a significantly higher concentration of retinol (0.4%) is required to attain similar outcomes as observed with topical retinoic acid, retinol triggers similar histological alterations (epidermal thickening and dermal ECM production) as retinoic acid. However, inappropriate or excessive use of topical retinoids or retinoic acid may also result in potential side effects. These commonly include skin dryness, redness, and peeling, which can cause discomfort. However, these side effects typically diminish over time as the skin adjusts to the product. Evidence suggests that HPR will induce fewer adverse side-effects than the other retinoids.
Long-term use of retinoids (studied for up to 2 years) have found beneficial effects to the skin throughout the treatment period, and a good safety profile. While most of the benefit is seen within 6 months following onset of the treatment, long term use can maintain the positive effects.
Summary
Topical retinoids (TR) are a safe and effective addition to one’s skin care routine, especially for aged skin. TR provides major benefits to the skin, including increased thickness of the epidermis and dermis, and enhanced blood flow to the skin. There are few side effects of retinoids, and if chosen properly, retinoid products, such as those that use HPR, are well tolerated by those with sensitive skin. Photosensitivity is not an issue, and their use with vitamin C/antioxidant products, such as those using gentle liposomal vitamin C (liposomal ascorbic acid), provides extra benefit.