Did you know scientists have discovered that topical sunflower seed oil helps to rebuild the stratum corneum and barrier function? Or that topical safflower oil can help to regrow hair and help to close wounds. Did you know that consuming seed oil, full of polyunstaurated fats, is healthier than eating coconut oil, which is 90% saturated fat. Consuming staurated fat leads to heart problems and dysbiosis, among other problems. Did you know that some seed oils, such as high oleic sunflower seed oil, tends to have higher stability than the high linoleic varieties of oils? Or that safflower seed oil contains extremely stable oleosomes? These are the reason why I formulate with these two oils. They provide essential oils (oils the skin needs to aquire to be healthy but are not made by the skin) and they provide numerous benefits to the skin. If the seed oils are extracted carefully, such as expeller pressed, and then formulated in a cold-process, the seed oils are of great benefit to the skin.
Listening to some unknowledgeable and outspoken people on TikTok, YouTube, including some pharmacists, or any of a number of podcasts, the oil extracted from plant seeds is poisoning us. RFK, Jr., who should have stuck with being an environmental lawyer, has jumped on this inane bandwagon. I think his cerebral arteries must be clogged with beef tallow (50% saturated fat) and advanced glycation end products from the fries he eats. Other people, such as the physician Mark Hyman are telling people to eat unhealthy coconut oil instead of seed oils – I guess he’s trying to drum-up business. Coconut oil induces inflammation and metabolic disorders, and a coconut oil- high fat diet has been found to cause dysbiosis associated with an increased risk of colorectal cancer. Further, diets rich in saturated fats, such as coconut oil, may contribute to mitochondrial dysfunction, protein aggregation, and neuronal degeneration. Recent studies (McCright et al, 2025) also find that saturated fats exacerbate asthma and promote lung myeloid cell inflammasome activation and IL-1β–mediated inflammation in mice and humans.
Instead of pseudoscience from RFK, Jr, try some science from Prof. Dr. Christopher Gardner, Ph.D. on a recent podcast. “It’s so odd that the internet has gone wild demonizing these things [seed oils],” said Dr. Christopher Gardner, Ph.D., a professor of medicine at Stanford University School of Medicine in California and a nutrition scientist at the Stanford Prevention Research Center. “They are not to be feared.” Dr. Gardner says seed oils contain high levels of omega-6 fatty acids, a polyunsaturated fat the body needs but cannot produce itself, so it must come from foods. Polyunsaturated fats help the body reduce bad cholesterol, lowering the risk for heart disease and stroke. The American Heart Association supports the inclusion of omega-6 fatty acids as part of a healthy diet. Studies of linoleic acid, found in seeds, finds the seed oils benefit cardiovascular function.
Seed Oils in Topical Skincare Products
Some seed oils, such as sunflower seed oil, are great for the skin. Sunflower seed oil helps to rebuild skin barrier function. In contrast to sunflower seed oil, topical treatment with olive oil significantly damages the skin barrier, and therefore has the potential to promote the development of, and exacerbate existing, atopic dermatitis.
Sunflower Seed Oil
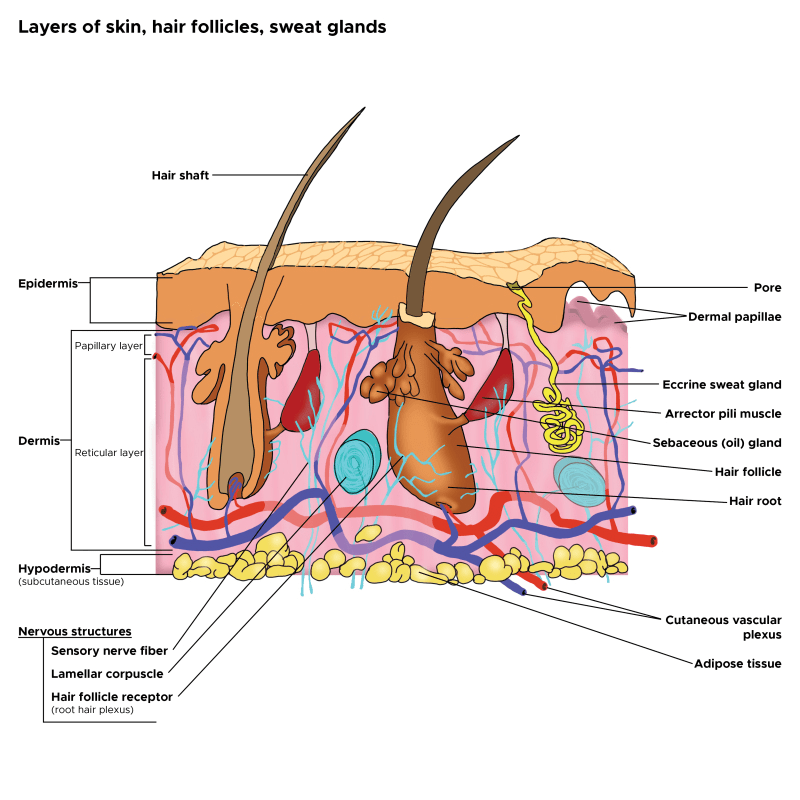
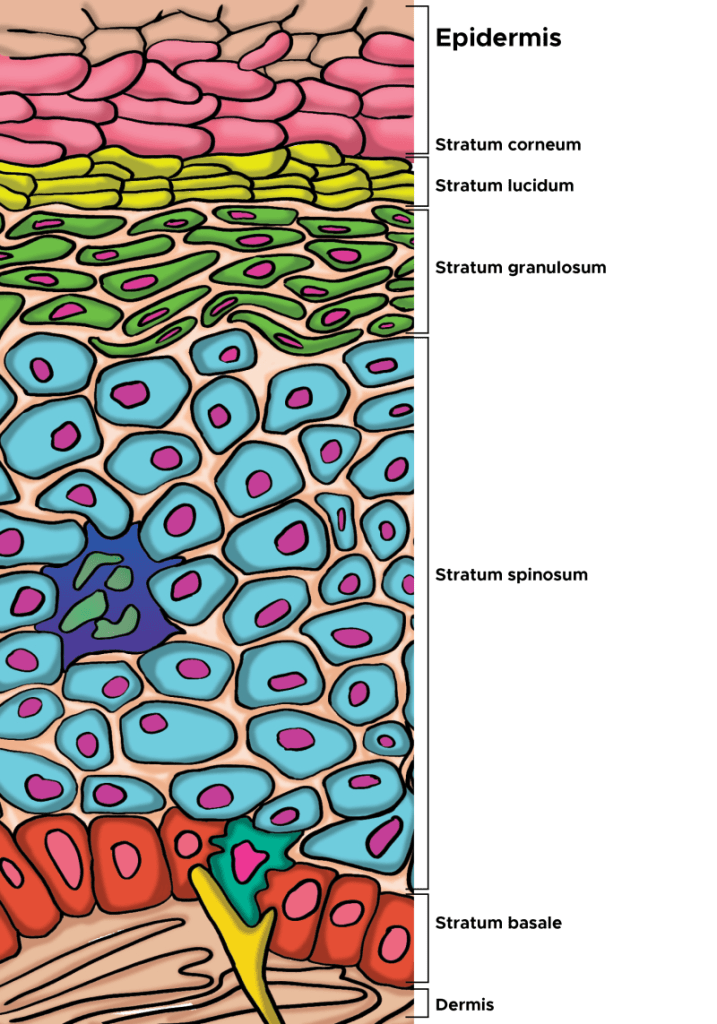
Notice sunflower seed oil (SFSO) is used by dermatologists at UCSF, such as Prof. Dr. Peter Elias, M.D. and his colleagues, in an inexpensive product for building the epidermis and barrier function: https://pmc.ncbi.nlm.nih.gov/articles/PMC9078150/. There are other products that work better, but they are more expensive because of ingredients like oleosomes, Triple Lipid Technology and Natural Mositurizing Factors, things that I’ll explain later. The product developed by Prof. Elias and colleagues features sunflower seed oil, something that is less expensive but provides benefit to barrier function. SFSO activates PPAR-alpha, which has numerous benefits in the epidermis (increased lipid production and lamellar body formation, and differentiation of keratinocyes) that help to rebuild natural barrier function. Sunflower seed oil contains oleosomes if cold-processed and not refined. Oleosomes are specialized plant organelles that protect the oil, and I’ll describe in the next section.
From Elias et al (2022): The putative mechanisms by which a topical optimised mixture improves permeability barrier homeostasis. In the mixture, petrolatum and lanolin instantly improve the permeability barrier, while glycerol improves barrier (stratum corneum, SC) hydration and accelerates permeability barrier repair. Linoleic acid in both sunflower oil and borage oils activates peroxisome proliferator-activated receptors (PPAR), resulting in increased production of lipids and antimicrobial peptides, and stimulation of lamellar body secretion and membrane maturation. Consequently, both permeability barrier and antimicrobial barriers are improved.
Safflower Seed Oil and its Oleosomes
I’ll also described the benefits of safflower seed oil (SSO), and the oleosomes contained within. SSO has antioxidant and antimicrobial activity, helping to heal wounds. The potential uses of SSO for skin care are under intense investigation given what is already known of this oil. For example, recent results indicate that SSO and its active compound acacetin can prevent UVB-induced MMP-1 expression, which leads to skin photoaging.
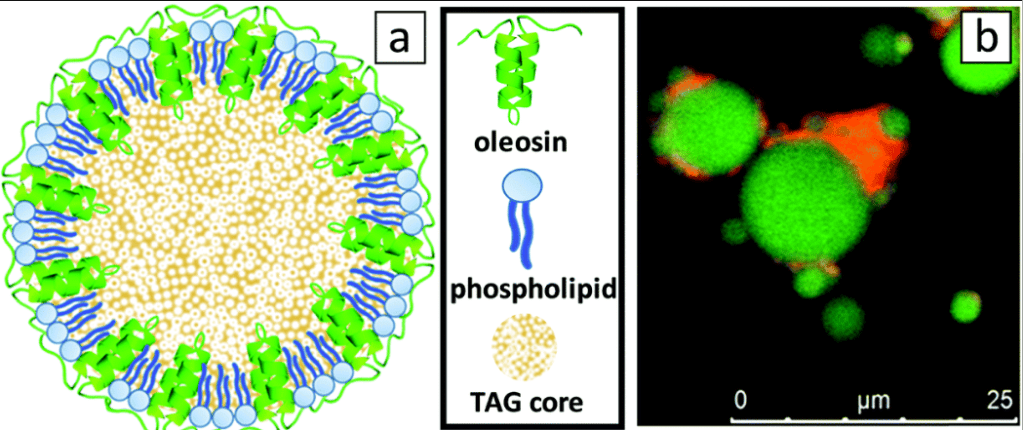
From Karefyllakis et al (2019): 2D-model of an oleosome with an emphasis on the configuration of the membrane, composed from a monolayer of phospholipids with the hydrophobic oleosin proteins anchored in the triacylglyceride (TAG) core (sizes not to scale), and (b) CLSM (confocal laser scanning microcope) image of SFO stained by Nile Blue showing lipids in green and proteins in red.
Safflower oleosomes are of interest in part because the plant seeds uniquely contain a large amount of oil bodies (oleosomes) and low water content, resulting in decreased hydrolytic properties and lower protein degradation. Within the oil, tocopherol or vitamin E occurs naturally. Looking at the evolution of plant seeds, the primary function of oleosomes is to safely store the seed energy source in the form of triacyglycerols (vegetable oil) during dormancy of the seed and then use it during germination, and to protect the seeds against environmental stressors. To achieve this, a sophisticated structure has evolved where oleosomes are equipped with a membrane that covers the triacylglycerols (TAGs) core, imparting physical and chemical stability. The membrane acts as a shield, preventing the oxidation of the TAGs. The membrane is dilatable and consists of a continuous monolayer of phospholipids that contains a number of proteins, mostly oleosins, embedded in the membrane. Triacylglycerols, also known as triglycerides, are a type of lipid composed of a glycerol molecule bonded to three fatty acids. They are the main constituents of body fat in animals and vegetable fats. Triacylglycerols serve as a crucial energy reserve, storing more than six times the energy of glycogen per gram. The seeds need this energy to germinate.
The oleosomes we use at NeoGenesis are naturally and sustainably extracted from the seeds of safflower (Carthamus tinctorius). The herbaceous non-GMO plant is cultivated and harvested in California, USA, without the use pesticides and with low water requirements. The manufacturer with whom we work, Sharon, uses a proprietary aqueous extraction cold process, comprising: grinding the seeds with aqueous medium, centrifugation and separating the liquids from the solids by centrifugation again before isolating the oleosomes. This process keeps the oleosomes fully intact, maintaining the micro-oil bodies as they occur naturally, with their full qualities and capabilities. Further, cold processing retains the antioxidants, vitamins and minerals. The result is an oil-in-water (o/w) emulsion with natural properties that provide many skin benefits. Biophysical studies of the oleosome have characaterized the oleosomes’ high physical stability, and have called for bioinspired construction of oil structures capable of protection and delivery of ingredients to the skin, all based on the remarkable evolutionary structure of the oleosome.
Sea Buckthorn Oil (Berries, Pulp, and Seeds)
Sea Buckthorn Seed Oil (SBSO), which typically contains the oil from the berries and pulp too, is another highly prized oil for skin care. One of the key reasons I use it in my topical skin care formulations is the high level, about 50%, of Omega-7 fatty acids. SBSO has been found to aid wound healing and increases telomerase activity, and decrease 3-nitrotyrosine. Inhibiting 3-nitrotyrosine (3-NT) is huge because 3-NT is a stress factor and acts as a neoantigen leading to the production of autoantibodies that can destroy skin tissue.
More than Omega-7, sea buckthorn (Hippophae rhamnoides) is valued for its diverse array of bioactive compounds. Cold-pressed extraction is important for retaining the full spectrum of these compounds. The SBSO is typically derived from various parts of the plant, including the whole berry, pulp, and seed, each yielding unique profiles of fatty acids, vitamins (A, C, and E), phytosterols, flavonoids, and carotenoids. SBSO, in particular, is rich in polyunsaturated fatty acids like linoleic acid (omega-6) and linolenic acid (omega-3), as well as the monounsaturated fatty acid palmitoleic acid (Omega-7). SBSO also contains a small amount of saturated fatty acid palmitic acid, monounsaturated fatty acid oleic acid, and trace amounts of myristic and stearic acids, along with minerals such as selenium, copper, zinc, and silicon. Together, this remarkable array of components in SBSO enhance the epidermis’ skin barrier function, structural integrity, and and anti-inflammatory properties, making SBSO a valuable therapeutic agent for conditions such as skin wounds, atopic dermatitis and psoriasis, or any skin condition with inflammation and compromised barrier function.
Other seed oils have been found to provide benefit too. Raspberry seed oil, for example, improve barrier function as measured by decreases of TEWL in human subjects, whereas the comparator oil, coconut oil, had no effect. Let’s stop denegrating seed oils!
Beneficial Seed Oils for Skin
| Oil | Key Components | Main Skin Benefits | Skin Types Best Suited For |
|---|---|---|---|
| Rosehip Seed Oil | Linoleic acid, α-linolenic acid, provitamin A (retinoids), tocopherols | Promotes skin regeneration, reduces scars and hyperpigmentation, improves elasticity | Dry, mature, scar-prone |
| Pomegranate Seed Oil | Punicic acid (omega-5), polyphenols | Strong anti-inflammatory and antioxidant activity, supports skin repair, calms redness | Sensitive, inflamed, aging skin |
| Black Cumin Seed Oil | Thymoquinone, linoleic acid | Antimicrobial, reduces acne inflammation, supports wound healing | Acne-prone, oily |
| Chia Seed Oil | α-linolenic acid, phytosterols | Improves hydration barrier, reduces trans-epidermal water loss, calms irritation | Dry, sensitive, eczema-prone |
| Hemp Seed Oil | Balanced omega-3 and omega-6, γ-linolenic acid | Regulates oil production, reduces inflammation, strengthens barrier | Oily, acne-prone, combination |
| Pumpkin Seed Oil | Zinc, tocopherols, phytosterols | Promotes firmness, antioxidant protection, may help with hormonal skin changes | Aging, combination |
| Sea Buckthorn Seed Oil | Palmitoleic acid, carotenoids, tocopherols | Heals damaged skin, boosts elasticity, protects against oxidative stress | Dry, sun-damaged |
| Raspberry Seed Oil | Ellagic acid, tocopherols, polyunsaturated fats | Antioxidant, anti-inflammatory, mild natural UV protection | Sensitive, aging, photo-exposed |
Summary
Bottom line, if you’re using coconut oil or olive oil on your skin, your not improving epidermal function, you can be degrading it. Switch to products using evidence-based, scientific knowledge to formulate their products – and, yes, seed oils, providing essential oils, can be great for the epidermis and improving barrier function. For example, if you use the NeoGenesis Barrier Renewal Cream, you’ll benefit from safflower oleosomes, combined with our Triple Lipid Technology (free fatty acids, ceramide, cholesterol) and Natural Moisturizing Factors (NMF) to rebuild the stratum corneum and barrier function. No other company features this combination of ingredients to rebuild the epidermis. And for those with moderate to severe barrier dysfunction, our new MB-2 product provides instantaneous barrier function without the use of petrolatum, along with 5 types of symbiotic bacteria important to rebuilding barrier function and inhibiting Staphylococcus aureus overgrowth, commonly found in skin with disrupted barrier function. One last thing, NeoGenesis S2RM, containing adipose mesenchymal stem cell secretome, helps to rebuild barrier function too!
For those with disrupted barrier function in conditions such as eczema, including atopic dermatitis, I recommend Skin Serum, which contains S2RM and glycerol, Barrier Renewal Cream, which contains oleosomes+ Triple Lipid Technology +NMF, followed by MB-2, containing a non-petrolatum occlusive+5 live symbiotic bacteria. There’s no better way to improve epidermal health and barrier function, and seed oils are part of the rebuild!.